Abstract
Introduction
Gut colonization with vancomycin-resistantenterococci (VRE) (specifically, Enterococcus faecium and E. fecalis) is common both before and after allogeneic hematopoietic cell transplantation (allo-HCT), and has been variably associated with VRE bloodstream infections. Clinical infections with intrinsically low-level VRE( E. gallinarum and E. casseliflavus), which have the chromosomally encoded vanC gene, are rare. Additionally, the clinical impact of pre-HCT gut colonization with these bacteria is unknown. In this study, we evaluated the outcome significance of pre-HCT colonization with E. gallinarum and E. casseliflavus, collectively named "intrinsics" herein.
Methods
We retrospectively reviewed the medical records of all adult and pediatric (>1 year old) allo-HCT recipients with available pre-HCT rectal swab or stool culture results at our institution (2011-2017). Second transplant recipients were excluded. SpectraTM VRE chromogenic agar medium (ThermoFisher Scientific) was used for species-level identification, and vancomycin E-test was used for MIC determination. Cases with ≥1 positive pre-HCT result for E. gallinarum or E. casseliflavus and no positive test for VRE or vancomycin-intermediate enterococci (VIE) were defined as intrinsics. Patients with no previous positive test for intrinsics or VRE/VIE, and with at least 2 negative tests for all these, were defined as controls. Due to the rare occurrence of colonization with intrinsics and the preponderance of pediatric patients with this condition, we used a matched-pairs design. Each intrinsic case was matched to a control using the following hierarchical criteria: (i) Diagnosis (malignant vs. non-malignant), (ii) disease risk (standard vs. high vs. non-malignant), (iii) donor type (matched sibling vs. matched unrelated donor vs. cord blood), (iv) conditioning intensity (myeloablative vs. reduced-intensity), and (v) age (± 10 years). The Prentice-Wilcoxon test was used to evaluate the matched pairs on the primary endpoints of overall survival (OS). For relapse and RFS, we excluded patients with non-malignant disorders.
Results
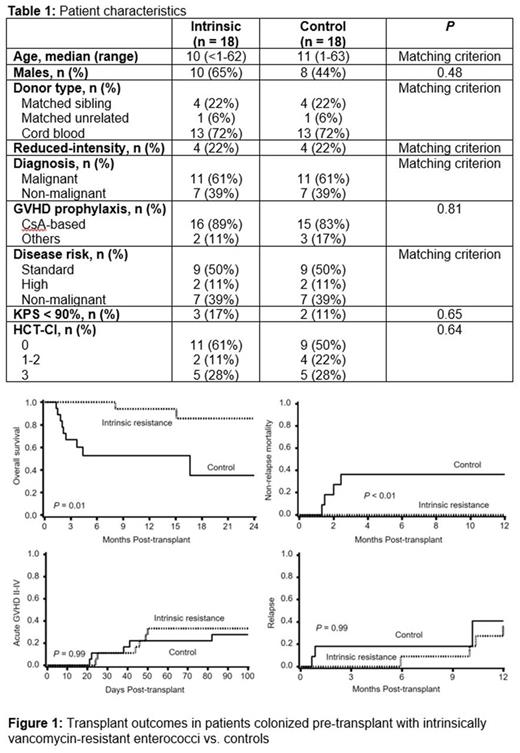
Table 1 shows the characteristics of the control group and intrinsics (n = 18 in each group). The groups were similar in all studied variables. The median follow up was 15 months. The intrinsic group showed a significantly higher 2-year OS of 86 [52-96]% vs. controls with OS of 35 [8-65]% at 2 years (P < 0.01, Figure 1). This remarkable difference in OS was due to a significantly lower NRM in the intrinsic group (0% vs. 36 [8-65]%, P= 0.01). Other transplant outcomes (GVHD and relapse) in each group were similar. Both deaths in the intrinsic group were due to relapse. In contrast, deaths in the control group were due to organ failure in 45%, relapse in 33%, infection in 11%, and GVHD in 11%.
Conclusions
In matched-pair analysis of intrinsically vancomycin-resistantenterococcivs. controls, we observed a remarkably lower NRM among patients colonized pre-HCT with E. gallinarum or E. casseliflavus .The mechanisms for this finding remain to be further explored. We hypothesize that in addition to vanC, these organisms have other genes that collectively contribute to establishment of a protective microbiome against various etiologies of early post-transplant NRM. This may occur as a result of beneficial microbial secondary metabolites that modulate the host immune system, or be consequent to colonization resistance against pathogenic organisms.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.